The following describe
how one would approach a fluorescein angiography in clinical practice.
In part II MRCOphth, you will normally be given a frame of fluorescein
angiography with characteristic pathology (usually with either hyper or
hypofluorescence or a combination).
A methodical approach to
angiogram will ensure that maximum information is gained from the investigation.An
accompanying colour fundus photograph is essential for meaningful interpretation,
along with relevant clinical information.
Changes in the appearance of abnormal
area through the 5 phases of the angiogram add extra information. For this
reason it is more meaningful to follow an abnormal feature through a sequence
of angiogram photographs, then to analyse each photograph separately.
Start with any striking abnormality
and describe this in detail:
-
Hypo/hyperfluorescent components
-
Intensity of lfuorescence and changes
with time
-
Area of fluorescence and changes
with time
a
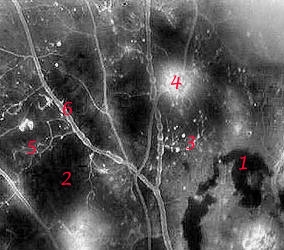
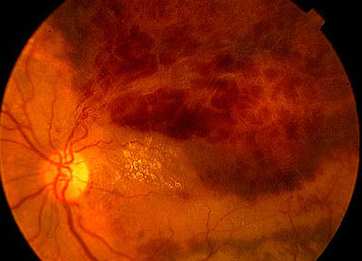
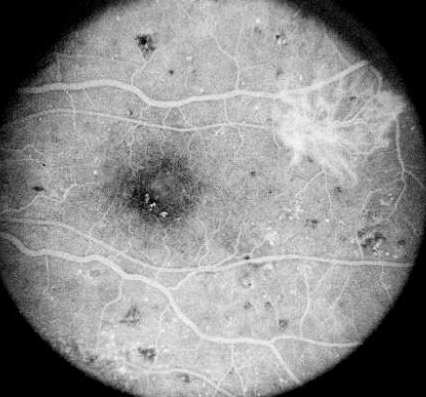
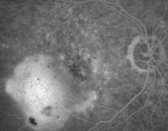
Diabetic retinopathy gives a combination of both hyper/
hypofluorescence. Several pathologies are seen in this
frame:
Hypofluorescence: retinal haemorrhage (1) and ischaemia
(2).
Hyperfluorescence: microaneurysms (3) and neovascularization
(4)
In addition, there are IRMA (5) between the retinal artery
and vein and venous beading (6) |
Where there are multiple
abnormalities, list these systematically. After commenting on all abnormalities,
run through an anatomical check list to ensure all feature have been included:
-
macula
-
optic disc
-
large retinal blood vessels
-
retinal capillaries
The following are common abnormalities
seen in fluorescein angiography
-
Timing -
arm to eye time and retinal circulation
may be prolonged if the cardiac output is low
or the carotid perfusion is reduced.
-
Abnormal dye distribution
-
area may be present in which fluorescence
is abnormally reduced (hypofluorescence)
or abnormally increased (hypofluorescent).
Summaries of
abnormal dye distribution
Hypofluorescence
-
Transmission defect (blood, pigment, hard exudates etc)
-
Filling defect (circulation abnormality)
Hyperfluoresence
-
Window defect (RPE defect)
-
Leakage of dye (SRNVM and new retinal vessels)
-
Pooling of dye (RPE detachment)
-
Staining of dye (damaged blood vessels; drusens)
-
Autofluorescence
|
Causes of hypofluorescece:
It can be caused by either the
blockage of light or inadequate circulation in areas of retina or
choroid:
1. Decreased
transmission
- blockage may be caused by the
accumulation of pigment, naevi,
exudate or abnormal material
(eg, the yellow flecks in patient with
Stargardt's disease)
- pre-retinal opaque structures
superficial to the retinal circulation
will mask both the retina
and choroidal circulation eg. preretinal
haemorrhage,
myelinated nerve fibres.
- prechoroidal opaque structures
deep to the retinal circulation but
superficial to the choroidal
circulation will mask only the choroidal
circulation for example:
blood - retinal haemorrhages in diabetic retinopathy and retinal vein
- subretinal blood from choroidal new vessels
exudates - hard
exudates
cotton wool spots
melanin- in hyperpigmented areas
of RPE; choroidal naevus (see below)
xanthophyll pigment - in the area
of the macula
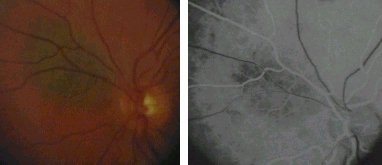
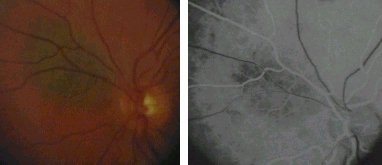
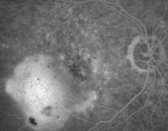
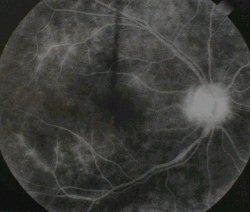
Choroidal naevus blocking the choroidal fluorescein in
the arterial phase. |
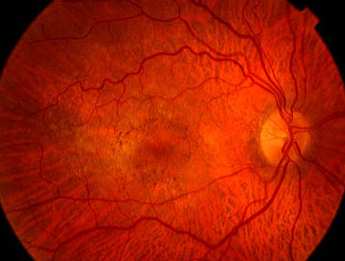
Central retinal artery occlusion with
non-perfusion of the retinal vasulature. |
Causes of hyperfluorescence
1. Window defects
of the RPE (for
example in RPE atrophy or macular
hole see
picture below)
- the RPE behaves as a
pigmented filter, reducing
transmission of fluorescence.
- areas of atrophy of RPE act as
windows through which the
fluorescence may be
seen more brightly. In ARMD,
fluorescein in the
choroidal circulation appears brighter
where the overlying
RPE is atrophic. These areas of
hyperfluorescence
are most prominent in the choroidal
phase, but persist
through out all phases of the angiogram.
 ... ...
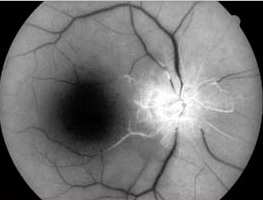
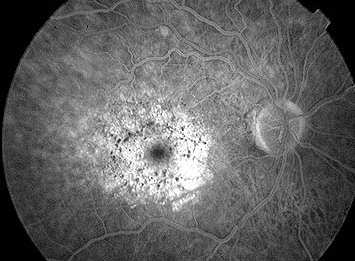
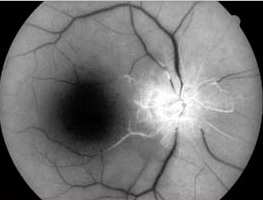
Left macular hole. There is left foveal hyperfluorescence
due to loss of the marking
effect of RPE cells. |
2. Leakage
of dye
- it occurs when there
is breakdown of the tight junction of
the RPE or the retinal endothelium.
3. Leakage with pooling
- if fluid is present
under the RPE or the sensory retina,
fluorescein may collect
in these spaces and cause pooling
of the dye resulting
in the characteristic angiographic
picture of serous
detachment of the RPE or of the sensory
retina.
- sometimes, dye may fail
to accumulate even in the
presence of apparent
fluid due to the fact that the fluid is
either no longer entering
the area or is collecting too slowly
for a sufficient concentration
fluorescein to be
photographed. RPE
detachment, central serous retinopathy
and cystoid macular
oedema are examples of leakage with
pooling.

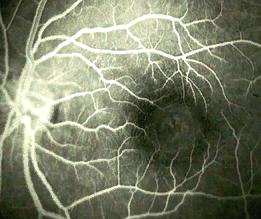
Cystoid macular oedema with
petalloid pattern in late phase. |
4. Leakage
with staining
- collagen absorbs fluorescein
dye causing staining which
persists after dye
has been cleared from the choroidal and
the retinal circulations.
For example profound ischaemia
and vasculitis both
lead to incompetence of retinal
endothelium tight
junction. Leakage of dye into the
connective tissue
of the blood vessels result.
- optic disc staining, staining
of the sclera, most evident at
the optic disc is
a normal angiographic feature. The dye is
derived from the choroidal
circulation, and staining is most
evident in the late
phase.
Par planitis showing staining of the blood vessels
and dye leakage at the optic disc. |
5. Drusen
present in age-related maculopathy
becomes stained by
absorbing
dye from the choroidal circulation.
Late phase. A leaking subretinal
neovascularization and staining of
the drusen. |
6. Leakage from
abnormal vessels
- choroidal and retinal
new vessels are structurally abnormal
and do not have intact
endothelial tight junctions. Fundal
tumours such as choroidal
malignant melanoma, have their
own blood supply which
may leak.
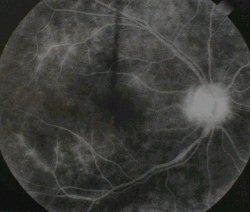
7. Autofluorescence
- optic disc drusen
is the classic example. They are visible
before dye injection.

Optic disc drusen |
|